Coronavirus and the Neurological Side Effects of COVID-19
Review of COVID-19
Coronavirus is a type of virus of which there are many different variations. The most well-known, of course, is COVID-19 which emerged in late fall/winter of 2019. The first case reported was caused by a coronavirus later named SARS-CoV-2 which may have originated in an animal and mutated (changed) into a variation that can cause illness in humans. In the past, several infectious diseases have been traced to viruses originating in birds, pigs, bats, and other animals whose eventual mutations have become dangerous to humans.
COVID-19 can be severe and has caused millions of deaths around the world as well as lasting health problems in some who have survived the illness.
Researchers have found that the coronavirus is spread through droplets and virus particles released in the air when an infected person breathes, talks, laughs, coughs, or sneezes. Tiny, infected particles can linger in the air and accumulate in indoor places where people tend to gather in large groups. This combined with poor ventilation increases the chance of infection.
Symptoms show up within 2 to 14 days of exposure to the virus and the infected person is contagious to others for 10 to 20 days, depending on the severity of their illness and condition of their immune system.
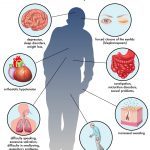
Classic Symptoms of a Coronavirus Infection
Cough, fever and/or chills, shortness of breath, sore throat, muscle or body aches, loss of taste or smell, diarrhea, headache, fatigue, nausea or vomiting, and congestion, or runny nose are some symptoms of coronoavirus infection.
Some people have a mild illness – much like a cold – and others have no symptoms at all. In some cases, though, COVID-19 can lead to respiratory failure and lasting lung, heart, or other system problems, or death.
Obtaining a Coronavirus Diagnosis
Diagnosis is difficult since many COVID-19 symptoms can be caused by other illnesses and some people do not have symptoms at all. At home tests are not always dependable, but if done correctly and the test result is positive you should assume you are infected.
The most accurate test is the molecular test – PCR (polymerase chain reaction), which is administered by medical professionals. Like the home test it is done with a nasal swab.
Treating COVID
Treatment depends on the severity of the infection. Mild illness responds to resting at home and taking medicine to reduce any fever. As mentioned on Johns Hopkins website, more severe cases may require hospitalization and treatment that might include intravenous medications, supplemental oxygen, assisted ventilation, and other supportive measures. It is obvious that if you have existing medical conditions, you should contact your physician as soon as possible to discuss what to do for treatment.
How Does COVID Infection Affect the Brain
Researchers have identified 4 ways COVID-19 may harm the brain, but each needs to be studied more deeply before any conclusions can be made.
- Severe infection
The virus may have the capacity to enter the brain and cause a severe and sudden infection. The virus’s genetic material was found in spinal fluid in cases reported in Japan and China. A case in Florida found viral particles in brain cells. This could occur due to the virus entering the bloodstream or nerve endings. The loss of smell in some COVID-19 cases might indicate that the virus entered through the olfactory bulb, which is located right above the nose and communicates information about smell to the brain.
- Immune system in overdrive
There is the possibility that the immune system goes into overdrive in an attempt to fight COVID-19, producing a “maladaptive” inflammatory response that may cause the tissue and organ damage seen in this disease – perhaps more than the disease itself.
- Chaos in the body
The third theory is that all the physiological changes induced in the body by COVID-19 – ranging from high fevers to low oxygen levels to multiple organ failures – contribute to, or account for, brain dysfunction, such as the delirium or coma seen in many of the severe cases.
- Blood-Clotting Abnormalities
The fourth way COVID-19 might affect the brain is the tendency for these patients to have a stroke. With a highly abnormal blood-clotting system in these patients, clots are more likely to form. Clots can form in veins deep in the body or in the lungs where they can cut off blood flow. A stroke could occur if a blood clot were to block or narrow arteries leading to the brain.
At Johns Hopkins, studies are being done by investigating selected cases, conducting the appropriate studies, and imaging, such as MRIs, electroencephalograms (EEGs) and samples of spinal fluid. It can be challenging to get these studies, since COVID-19 patients can be extremely weak and even confused. There needs to be a balance in treating their immediate needs with information gathering to better understand how we can help fight the virus in others who may develop this condition in the future.
Neurology Associates – Helping Patients Navigate Neurological Damage of Coronavirus
Physicians continue to deal with the fallout from COVID-19 and the long-term damage it causes in some patients. If you continue to have symptoms from a coronavirus infection, especially ones that may be considered neurological, contact Dr. Dulai’s office to schedule an appointment. He can review your case and offer treatment options.
Reference: How Does Coronavirus Affect the Brain? | Johns Hopkins Medicine